Introduction
Back pain is a common complaint, but when does it indicate something serious like a herniated disc? Whether you’re lifting groceries or sitting at a desk, sudden or chronic discomfort can leave you wondering: Is this just a strain, or could it be a spinal issue? In this guide, we’ll unpack herniated disc symptoms, expert-backed advice, and steps to protect your spine.
Understanding Herniated Discs: What Happens Inside Your Spine?
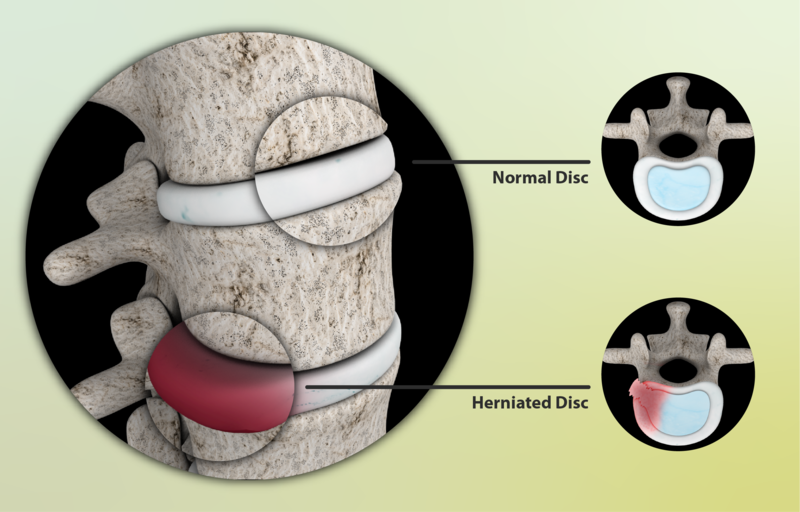
Your spinal discs act like shock-absorbing cushions between vertebrae. Imagine a jelly doughnut—a tough outer layer (annulus fibrosus) surrounds a soft, gel-like center (nucleus pulposus). A herniated disc occurs when the “jelly” pushes through a tear in the outer layer, potentially irritating nearby nerves.
Common Causes:
- Age-related wear and tear
- Improper lifting techniques
- Sedentary lifestyle or poor posture
- Trauma from accidents or sports
Is It a Herniated Disc? Key Symptoms to Watch For
Not all back pain points to a herniated disc, but these signs suggest it’s time to investigate:
1. Radiating Pain: Sharp, burning pain that travels to your buttocks, thighs, or calves (sciatica).
2. Numbness or Tingling: Pins-and-needles sensations in the legs or feet.
3. Muscle Weakness: Difficulty lifting objects or walking due to weakened muscles.
4. Worsening Pain with Activity: Discomfort intensifies when bending, coughing, or sitting for long periods.
Red Flags
- Loss of bladder/bowel control
- Severe weakness in both legs (seek immediate care)
How Do Experts Diagnose a Herniated Disc?
Diagnosis typically involves:
- Physical Exam: Tests like the straight leg raise to check nerve irritation.
- Imaging: MRI or CT scans to visualize disc damage.
- Neurological Assessment: Evaluating reflexes and muscle strength.
Treatment Options: From Conservative Care to Surgery
1. Non-Surgical Approaches:
Rest & Activity Modification: Avoid heavy lifting; gentle movement aids recovery.
Physical Therapy: Strengthen core muscles to support the spine.
Medications: Anti-inflammatories or muscle relaxants for pain relief.
2. Advanced Treatments:
Epidural Steroid Injections: Reduce inflammation around nerves.
Surgery (Last Resort): Discectomy or microdiscectomy to remove herniated material.
Preventing Herniated Discs: Expert-Backed Tips
Practice Proper Posture: Keep your spine aligned while sitting/standing.
Lift Smartly: Bend at the knees, not the waist.
Stay Active: Strengthen core muscles with exercises like planks or yoga.
Maintain a Healthy Weight: Reduce pressure on your spine.
When to See a Doctor
Consult a healthcare provider if you experience:
– Pain lasting >2 weeks
– Numbness/weakness in limbs
– Bowel/bladder dysfunction (emergency)
FAQs About Herniated Discs
Q: Can a herniated disc heal on its own?
A: Yes! Many improve with rest and physical therapy within 6 weeks.
Q: Herniated vs. bulging disc—what’s the difference?
A: A bulging disc protrudes without rupturing; a herniated disc has a tear.
Q: Best sleeping position for disc pain?
A: Side-sleeping with a pillow between knees relieves spinal pressure.
Conclusion
While back pain is often minor, recognizing herniated disc symptoms early can prevent complications. Listen to your body, prioritize spine-friendly habits, and consult a specialist if red flags arise. Your spine is your lifeline—protect it!
